Join My List To Get The Full Guide
Understand Significance
Do Your Research
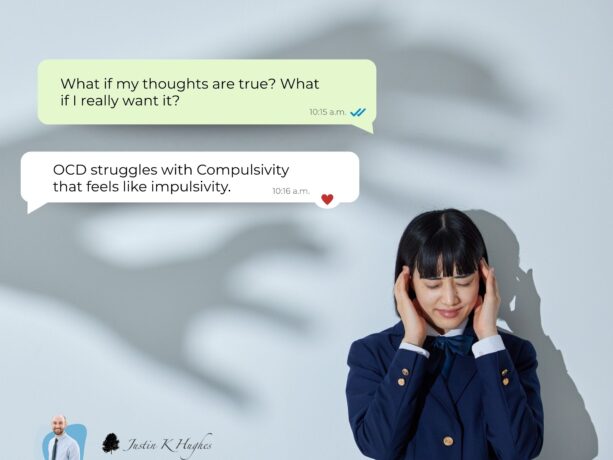
Make the Unseen Seen
Be Realistic With Expectations
Reinforce! Validate!
Support: Don’t Accommodate or be Emotionally Explosive
Make Space for your Own Growth and Boundaries
Relapse Prevention
Practical Tools for You
I often have my parents and significant others complete several documents and incorporate various tools. Each situation will vary, but commonly I use:
- Family Accommodation Scale (FAS)
- Hierarchy– Filling out a Hierarchy based on how difficult you think it would be for your loved one to accomplish said task without compulsion. Communicating with them and clarifying expectations and needs can really help in being realistic.
- Log
- Track/Monitor your observations:
- Track/Monitor your observations:
- Support Group / Therapy
- Some of my favorite stories, tools, and resources can be found on my ever-expanding page for OCD.
You Rock!!!
Get the Guide FREE by Joining a List!!!!
 References:
References:Calvocoressi, L., Lewis, B., Harris, M., Trufan, B. S., Goodman, W. K., McDougle, C. J., & Price, L. H. (1995). Family accommodation in obsessive compulsive disorder. American Journal of Psychiatry, 152, 441-443.
Depression and Other Common Mental Disorders: Global Health Estimates. Geneva: World Health Organization; 2017. Licence: CC BY-NC-SA 3.0 IGO.
Gillihan, S. J., Williams, M. T., Malcoun, E., Yadin, E., & Foa, E. B. (2012). Common Pitfalls in Exposure and Response Prevention (EX/RP) for OCD. Journal of obsessive-compulsive and related disorders, 1(4), 251-257.
What You Need To Know About Obsessive Compulsive Disorder. (n.d.). Retrieved February 2, 2020, from https://iocdf.org/wp-content/uploads/2014/10/What- You-Need-To-Know-About-OCD.pdf





Thanks
You are welcome!!!